Hear better with Jabra Enhance
With our advanced hearing aids and recommended expert care, you'll be hearing better in no time.

What you get with Jabra Enhance Select
High-tech hearing aids
Nearly invisible, Enhance Select hearing aids are Bluetooth-enabled, and offer 360-degree sound.
Convenient follow-up care
With our Premium Package, connect with our Audiology Team whenever you need via our easy-to-use app.
Incredible value
Everything you need for better hearing — all for as low as $995 per pair. Financing also available.
FSA and HSA cards accepted
100-day risk-free trial
Try Enhance Select hearing aids for 100 days. If you're not fully satisfied, we'll refund your entire order.

Proven Success
90% of customers using Enhance Select Premium report hearing better*
- 95% report hearing friends & family better
- 95% report asking others to repeat themselves less
- 95% report hearing the TV better
- 93% report hearing better at work
- 90% report hearing better in restaurants
*This data comes from all results of our 2023 Client Oriented Scale of Improvement tool. .

How it works
Take the online hearing test
See if you're a candidate for Enhance Select hearing aids. The recommended test is free, quick, and designed by audiologists.
Hearing aids delivered to your door
Your new hearing aids work right out of the box, whether you choose custom-programmed or preset for common types of hearing loss.
Enjoy 3 years of convenient follow-up care
With our Premium Package, our Audiology Team works with you remotely to improve your hearing.
Hearing aids for every budget & lifestyle
Everything you need for better hearing

Advanced hearing aids
High-quality devices with natural sound and Bluetooth streaming. *Direct stereo streaming is available for Apple devices across all our current Enhance Select models and previous models. Most Androids support direct streaming for our current Enhance Select models, while some Androids require an accessory. Close
Easy-to-use mobile app
Control and customize your hearing aid settings, stream music, and take calls.
Dedicated Audiology Team
With our Premium Package, get a 3-year comprehensive virtual care plan with our Audiology Team (aka no office visits).
- NewEnhance Select 300Excellent even in the most complex listening situations, like hearing multiple people at a loud party.$1,795 - $1,995

or as low as $58/mo per pair* - Enhance Select 100Great for everyday listening including tricky listening situations, like a conversation at a restaurant.$1,395 - $1,595
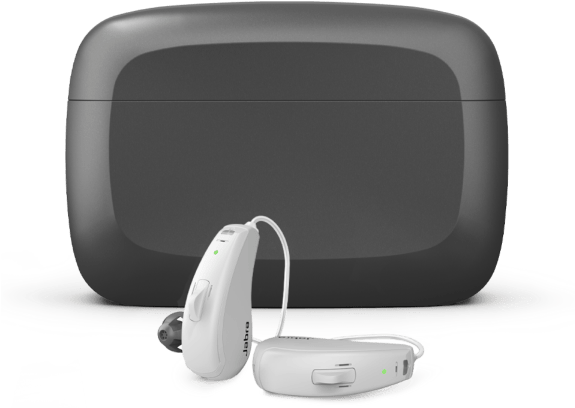
or as low as $46/mo per pair* - Enhance Select 50RWorks well in quieter situations, like one-on-one conversations and watching TV at home.$995 - $1,195

or as low as $33/mo per pair*
Buy now, pay later
As low as 0% APR and $0 down* with
Hear your life as it happens
The Select 300 enhances your hearing experience with 3 advanced key features
Hear your life as it happens
The Select 300 enhances your hearing experience with 3 advanced key features

Date night? Hear more conversations, fewer clattering dishes.
Get personalized care with our Premium Package
Programmed for you
Hearing aids custom-programmed to your unique hearing needs based on your online test results or audiogram.
Care from your couch
Video chat with a licensed hearing specialist about your hearing and hearing aids, as often as needed.
Adjustments made by experts
If you're having an issue, our Audiology Team will tweak your hearing aids via the app, from anywhere.
Your ears are in great hands
Jabra Enhance's audiology leadership and advisory board are globally recognized and trusted experts in hearing research, care treatment, and technology.
Audiology Dream Team

Our Head of Audiology Research, was formerly the Director of Research at the US Army Audiology & Speech Center. His work in hearing research has improved the lives of people around the world.
Our Head of Clinical Audiology, , received her Doctor of Audiology degree from St John's University. She's deeply committed to delivering high-quality care and education to patients on a daily basis.
Dr. Callahan leads our in-house team of licensed Audiologists and Hearing Aid Dispensers — innovators in the field dedicated to delivering exceptional care to customers across the country.
The reviews are in
We've selected a few reviews from customers who love what we do.
All reviews come from customers who purchased our Premium Package or equivalent, and completed an orientation within 30 days of purchase.
Company and model names have been updated to reflect our transition to Jabra Enhance and Enhance Select models.
Do I really have 100 days to try Enhance Select hearing aids?
What happens if the hearing aids don't work for me?
How do I connect my hearing aids to my phone?
How do you tune the hearing aids remotely?
Reach out to our team for help understanding if Enhance Select is right for you. No pressure, just trained professionals ready to talk. Or, visit our FAQ page for detailed info about our hearing aids, pricing, follow-up care, and more.